Gynaecological surgery can be confusing, emotive and sometimes complicated. Non-childbirth-related operations include myomectomy, hysterectomy, and pelvic floor repair.
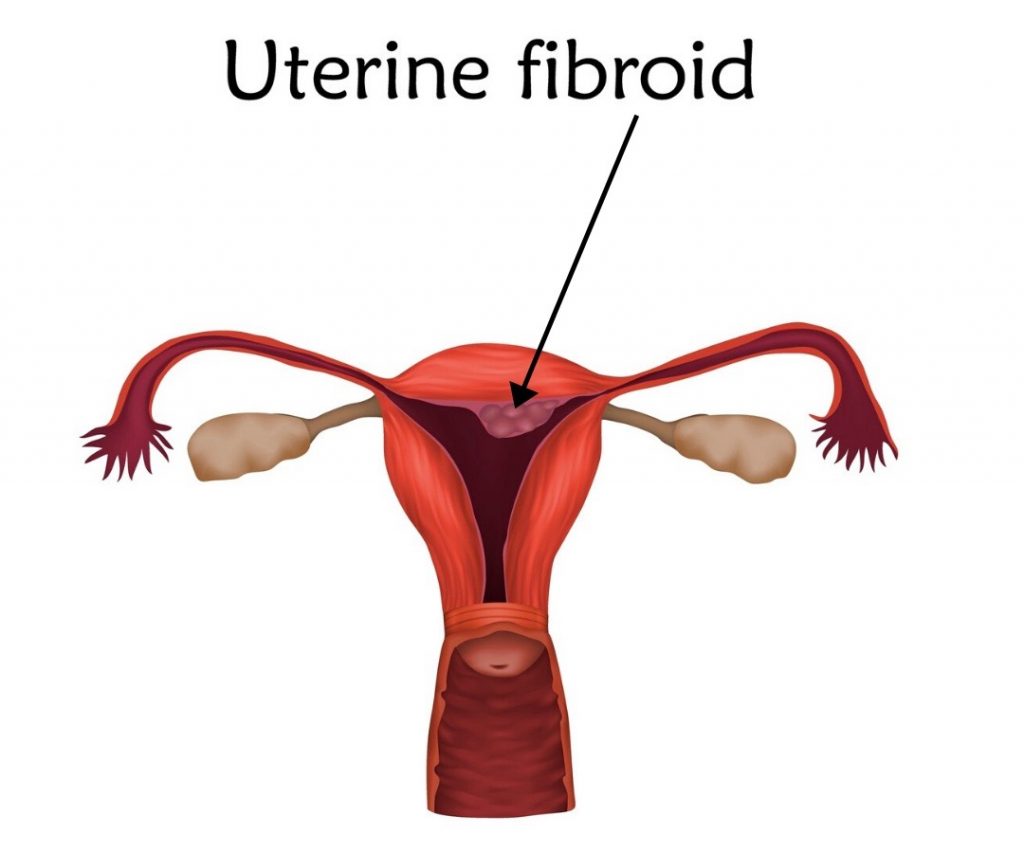
Myomectomy is the surgical removal of uterine fibroids which are benign (non-cancerous) growths that originate from the muscle of the womb. They can occur anywhere in the uterus; estimates suggest up to 80% of all women have fibroids.
This diagnosis often comes with the advice that patients can watch and wait, which is fine if they are not affecting daily life, as many will shrink at or around the menopause. However, even small fibroids can cause problems; they can disrupt the blood supply to essential structures in the pelvis, cause infertility, result in pregnancy difficulties or C-section deliveries. Uterine fibroids result in various symptoms, including:
- Heavy menstrual bleeding
- Anaemia and tiredness
- Severe pelvic pain
- Frequent urination
- Pain in the legs and back,
- Pelvic pressure and swelling of the abdomen
- Pain with intercourse
- Constipation
- Blood clots in the legs and pelvis
Treatment options
There are non-surgical options that aim to shrink fibroids and others designed to manage the symptoms, but many women will require surgery to resolve their fibroids symptoms. It’s one of the most common procedures carried out in gynaecological departments.
In women 45 years or older, or when fertility is no longer a viable option, some (too many) gynaecologists do not recommend or offer a myomectomy. In these cases, women will usually be told that a hysterectomy is a ‘better and final solution’ because it avoids the need for future surgery because fibroids can regrow.
Surgical options
Myomectomy and hysterectomy have a wide range of surgical options; including laparoscopic or keyhole approaches. More traditional open incisions and newer robotic techniques. Each procedure has different incision lengths, postoperative risk factors, and recovery outcomes.

Laparoscopic or keyhole approaches are often not suitable for the removal of large fibroids as the surgery can involve severe bleeding and other complications. It is also worth noting that laparoscopic procedures require a more skilled surgeon and can take more time, so some hospitals will advise women to opt for an open approach due to these constraints. However, in consultation with the surgical team involved women’s individual health concerns, beliefs and desire to have children should be the basis of surgery to remove fibroids.
Did you know that all keyhole procedures require patients to sign a consent form that permits the surgical team to switch to an open operation (abdominal incision) or perform a hysterectomy if the operative bleeding is extreme or there are other complications?
This news is often a worry as women can feel they have less control over their surgical outcome, some who have experienced this tell me they didn’t know this beforehand, so it was shocking news on waking from the anaesetic. It is essential to discuss with your surgeon in advance what this means for you. Fibroids can be problematic, and their removal requires a skilled surgical hand. When speaking to any doctor about fibroid removal surgery. If you are considering the surgical removal of fibroids, it’s essential to feel confident you are in the best hands so get informed about your options and ask the most appropriate questions.
Hysterectomy surgery can be complex in that there are different operations with many surgical approaches — all with differing recovery outcomes and postoperative risk factors.
Types of Hysterectomy
- Subtotal hysterectomy: involves the removal of the upper portion of the uterus, while the cervix and ovaries remain.
- Total hysterectomy: involves the removal of the uterus and the cervix.
- Radical hysterectomy: involves the removal of the uterus, cervix, fallopian tubes and ovaries.
Suggestions
Ask for any discussions and decisions about your surgery to be recorded in your notes and ask a copy if it would be helpful. Also, you can write your wishes on your consent form (there is space on the back page for this), some surgeons will ask you to do so as a matter of good practice. For example, “if a hysterectomy is necessary I do not consent for the removal of my cervix or ovaries unless its to preserve my life”. (unless you at high risk for cancer this should not be an issue). Note the medical term for the removal of both ovaries is bilateral oophorectomy.

Why the fuss?
There are many reasons to request this, including;
- The fact the cervix provides support for the bladder, and therefore the risk of prolapse reduced when it left in place.
- Many women report more enjoyable post-surgical sexual relations with their cervix intact.
- Keeping the ovaries avoids women crashing into the menopause. However, they are likely to fail within six months of the surgery as the ovaries get some of their blood supply from the uterus, but it will be a gentler process.
- Some women find it unacceptable to remove healthy organs.
Please take advice on your benefits and risks.
Questions to ask before any non-urgent surgery
A significant part of my work involves pre-surgery support, and post-surgical rehabilitation, which means I talk with people about their upcoming operation and the steps that may be useful before and afterward for a smooth recovery and stress-free rehabilitation.
I’m a massive fan of taking a list of questions and recording the answers in clinical or medical situations. Appointments are often time-constrained and stressful or involve lots of technical or medical language which can be overwhelming or simply a memory hurdle.
Asking questions does not mean you are challenging your doctor’s expertise or being disrespectful. All health professionals, including surgeons, want their patients to understand the procedure they’ve recommended to give informed consent. They also want you to know what to expect, so ask questions until you are comfortable with the process, the surgeon, the facility, and the aftercare.

Here are some suggestions
- Why do I need this surgery?
- What type of surgery are you recommending and why?
- Statistically, what is the success rate for this surgery?
- What is your success rate?
- Are there any non-surgical options that would be effective?
- How long will the surgery take?
- What are the risks?
- What is the risk/benefit ratio of an excellent surgical outcome?
- What are the long-term consequences of the proposed procedure?
- What are the side effects, potential risks, and complications of the surgery?
- Please explain the risks and how they relate to me.
- What if, during my surgery, you encounter a different issue than you expected?
Practicalities
- How long is the hospital stay?
- Will I be in pain after the surgery, and for how long?
- How do you manage the pain in the hospital?
- Will I be sent home with pain-relieving medications?
- What are the possible side effects of these prescriptions (e.g. constipation, drowsiness, etc.)?
- How do I best prepare for my surgery?
- What post-surgery advice can you give me now?
- What expectations do you have for my recovery?
Post-surgery
- Whom can I call if I have questions after being discharged?
- What symptoms would justify immediate medical attention?
- What kind of help will I need when I return home?
- How long will I be out of work?
- What limitations will I have after surgery and for how long?
- When is it safe to resume sexual relations?
- When can I drive again?
- What types of activities will I need to avoid doing after the procedure, and for how long?
- How often will I see you after my surgery?
Rehabilitation
- What post-surgery advice can you give me now?
- What rehabilitation will I need and for how long?
Plus, It’s always worth asking these just to see how they react.
- If I want to get a second opinion, can you recommend a surgeon?
- What would you recommend if I were your friend, would you suggest the same operation?

For NHS patients
Did you know that some surgeons only do a small part of the operation while others do the whole thing? If another surgeon is required, there may be a good reason, e.g. another skill set is needed, or it’s a teaching hospital. It may be worth asking:
- Do you perform the whole procedure?
- Will any students/other surgeons be doing any parts of the operation? If yes, who are they and what are their qualifications and how closely will they be supervised?
Summary
The prospect of any gynaecological surgery can be upsetting and worrying but an experienced patient-centered surgeon will understand your need for clarification and those with excellent results should be happy to answer all your questions. Any defensiveness by the surgeon or their team when you ask these types of questions should raise concerns, and perhaps prompt seeking a second opinion.
Next time: Pelvic floor repair surgery.







