Coeliac disease is a lifelong autoimmune condition triggered by a reaction to gluten. It’s surprisingly common, affecting 1 in 100 people, but many are living with the condition undiagnosed.
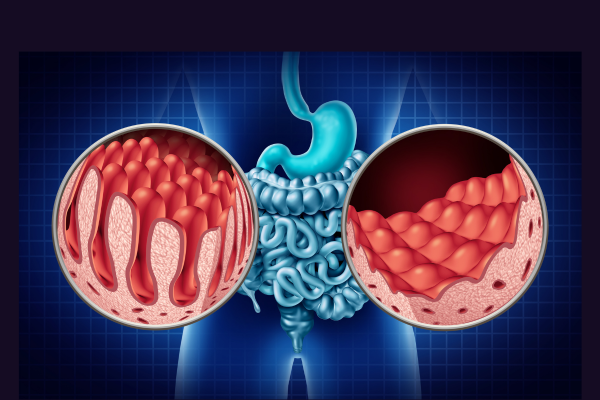
This disease was first described way back in the first century AD by a Greek physician named Aretaeus of Cappadocia, who identified it as a condition of the abdomen. In coeliac disease, eating foods containing gluten causes the lining of the small intestine to become damaged; it can also affect other parts of the body.
So, what is gluten?
Gluten is a protein found in wheat, rye, and barley, and for some people with coeliac disease, oats can also be a problem. If you have coeliac disease, eating gluten damages the lining of your small intestine and can cause issues in other parts of your body. The good news is that there are plenty of gluten-free options available nowadays, from bread and pasta to entire cookbooks dedicated to gluten-free baking. Many restaurants even offer gluten-free menus, making it easier than ever to manage this condition
Busting Common Myths
- Coeliac disease is not a food allergy or an intolerance.
- You don’t have to be underweight to have it.
- You can’t grow out of having coeliac disease.
- Some coeliacs are also affected by eating foods containing oats.
Who can get Coeliac disease?
Anyone can develop coeliac disease, regardless of age, gender, or ethnicity. It can start in infancy when cereals are introduced, during childhood, or at any point in adulthood. Unfortunately, delayed diagnosis is common, with the average time to diagnosis being around 13 years. This might explain why people aged 40-60 are most frequently diagnosed.s

Recognising the Symptoms
The symptoms of coeliac disease can vary widely from person to person, and they can range from very mild to severe. Here are some common symptoms:
- Recurrent stomach pain, cramping or bloating
- Occasional or severe diarrhoea
- Excessive wind and constipation
- Unexplained or persistent nausea and vomiting
- Deficiencies in Iron, Vitamin B12 or folic acid
- Fatigue or tiredness
- Unexpected weight loss in some people
- Mouth ulcers
- Skin rash (*Dermatitis Herpetiformis)
- Problems with tooth enamel
- Low mood or depression
- Liver abnormalities
- Repeated miscarriages
Complications of coeliac disease
Because the symptoms of coeliac disease are so variable, it’s often diagnosed late, sometimes many years after the onset of symptoms. This can lead to several complications:
- Neurological Issues: About half of newly diagnosed patients have neurological symptoms like ataxia (balance problems) and neuropathy (numbness and tingling).
- Bone Health: Untreated coeliac disease can lead to osteoporosis due to chronic nutrient malabsorption.
- Lactose Intolerance: Damage to the gut can lead to lactose intolerance, making diagnosis even trickier.

Diagnosing Coeliac Disease
Coeliac disease is often mistaken for irritable bowel syndrome (IBS) or other digestive issues. The initial symptoms can be similar, and there’s a general lack of awareness in many general practices. Remember, IBS rarely starts after age 50, so if you’re older and experiencing symptoms, consider getting tested for coeliac disease.
Tests and investigations
Diagnosis typically involves an antibody blood test and a biopsy of the gut lining. It’s crucial to keep eating gluten while being tested to ensure accurate results. Additional blood tests may check for nutrient deficiencies, and older individuals might need a DEXA scan to assess bone density.
Non-Coeliac Gluten Sensitivity:
Some people experience gluten-related symptoms without having coeliac disease, as they don’t show the typical antibodies or gut damage.
NICE guidance
The National Institute for Health and Care Excellence (NICE) recommends testing for coeliac disease if you have:
- Persistent unexplained gastrointestinal symptoms
- Prolonged fatigue
- Unexpected weight loss
- Severe or persistent mouth ulcers
- Unexplained iron deficiency anaemia or vitamin B12/folate deficiency
- Type 1 diabetes (at diagnosis)
- Autoimmune thyroid disease (at diagnosis)
- Irritable bowel syndrome (especially in older adults)
- A first-degree relative with coeliac disease
Treatment: Living with Coeliac Disease
There is no cure for coeliac disease, but it can be managed with a strict gluten-free diet. It’s important to avoid cross-contamination, as even tiny amounts of gluten can be harmful. Many supermarkets now stock gluten-free foods, and some are available on prescription. Cookbooks and restaurant options make it easier to maintain a varied and enjoyable diet.

Top Kitchen Tips from Coeliac UK
- Use separate cooking utensils for gluten-free food.
- Clean grills and use separate toasters or toaster bags.
- Use different breadboards and separate condiments to avoid cross-contamination.
Final Note
If you suspect you might have coeliac disease, don’t change your diet without consulting a doctor. It’s important to keep eating gluten while being tested to ensure accurate results.
Disclaimer
This blog is for informational purposes only and should not replace professional medical advice, diagnosis, or treatment. Always seek the guidance of a qualified health provider with any questions you may have regarding a medical condition.
SaveSave
SaveSave
SaveSave
SaveSave
SaveSave
SaveSave
SaveSave
SaveSave







