If you’ve been living with persistent back or neck pain that isn’t responding to hands-on treatment, medication, corrective exercise, or lifestyle changes, you might have been offered a spinal injection as a treatment option, but is that the right next step for you?
Spinal injections are often recommended for conditions like sciatica, herniated discs, and arthritis in the spine. One of the most common questions I hear from patients and in my classes is, “Should I go for it?”
Like any treatment, spinal injections have their pros and cons. It’s important to understand what they do, what risks they carry, and what side effects you might face before making a decision. Sadly, in today’s busy healthcare system—both NHS and private—patients don’t always get all the information they need. And when they do, it can be a bit overwhelming to take in.
Let’s take a closer look to help you figure out if a spinal injection could be the right choice for you.
Spinal Injections: The Inside Scoop
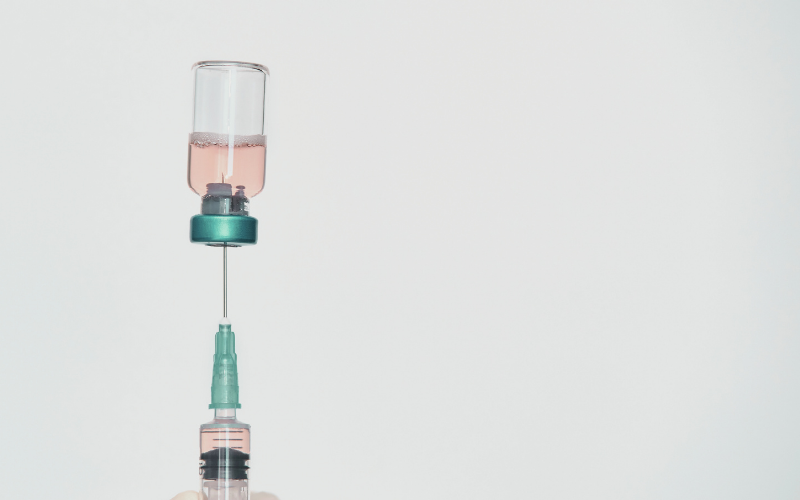
Spinal injections are used to reduce pain and inflammation; typically, they contain a mix of:
- Steroids – to reduce inflammation.
- A local anaesthetic – to numb pain.
Types of Spinal Injections
There are three main types of spinal injections:
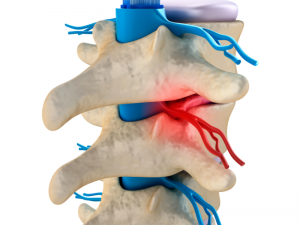
- Epidural steroid injections (ESI’s) – the most common and used for nerve pain like sciatica.
- Facet joint injections – for arthritis-related back pain.
- Nerve block injections – to “switch off” pain signals from specific nerves.
-
Sacroiliac Joint Injections: Injected into the sacroiliac joint, which connects the spine to the pelvis, to reduce pain and inflammation.
-
Radiofrequency Ablation: A minimally invasive procedure that uses heat to damage nerve tissues to reduce pain.
-
Regenerative Therapy Injections: These injections use the body’s own growth factors to accelerate the natural healing process.
-
Discography: A diagnostic procedure where contrast dye is injected into one or more spinal discs to identify the source of back pain.
The Benefits of Spinal Injections
-
Pain Relief
Many people feel relief within a few days or weeks, with the effects sometimes lasting for months. However, for some, the relief may be shorter-lived, and repeat injections may be needed. -
Helps You Get Moving Again
Once the pain is under control, it’s easier to get back to exercising, mobilising, and strengthening your body. This not only helps prevent future issues but also allows you to benefit more from hands-on treatments or physical therapy -
Can Delay or Avoid Surgery
If surgery isn’t your first choice, spinal injections can provide a less invasive option to manage your pain and give other treatments a chance. -
Helps Identify the Source of Pain
If doctors aren’t sure what’s causing your pain, a spinal injection can serve as a useful diagnostic tool. If it brings relief, it can help pinpoint the exact area of discomfort.
The Risks of Spinal Injections
While spinal injections can be life-changing for some, they’re not risk-free. Here’s what to consider:
1. The Relief Might Not Last – Some people feel great after an injection, but for others, the effects wear off quickly or don’t work at all. There’s no way to predict how you’ll respond.
2. Potential Side Effects
- Mild and temporary soreness at the injection site.
- A ‘flushed’ or warm feeling from the steroids.
- Leak of cerebrospinal fluid (not common), which may result in a headache.
- Soreness, bruising, and bleeding at the injection site.
3. Rare But More Serious Risks
- Infection – uncommon but possible.
- Nerve damage – rare, but a misplaced needle could cause irritation or weakness.
- Bleeding – especially if you take blood-thinning medication.
- Bone thinning – repeated steroid injections can weaken bones over time.
4. They Don’t Work for Everyone – Steroid injections are most effective for pain caused by inflammation. Some people only get mild or short-term relief.
How Long Does Pain Relief Last?
That’s a big and difficult one to answer; the duration of pain relief varies from person to person. Some key factors include:
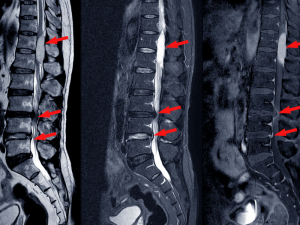
- The underlying condition: Injections work best for inflammation-related pain, such as nerve compression from a herniated disc or arthritis. Structural issues may not respond as well.
- The severity of the problem: Advanced degeneration or nerve damage may lead to shorter-lasting effects.
- Individual response to steroids: Some people respond well to steroid injections, while others experience little or no relief.
- Lifestyle and activity levels: Staying active, doing rehab exercises, and maintaining a healthy weight can prolong the benefits.
- Repetitive strain or ongoing aggravation: If activities continue to irritate the spine, relief may not last as long.
- Injection technique and accuracy: The precision of the injection (often guided by X-ray or ultrasound) can affect how well it targets the problem area.
Who Is an Ideal Candidate for Spinal Injections?
Spinal injections are typically recommended when:
- Pain is moderate to severe and affects daily life.
- The pain has not improved with manual therapy, rehab exercises, medication and lifestyle changes.
- Imaging (MRI or CT scan) shows nerve compression, inflammation, or joint degeneration that matches the pain pattern.
- You are not ready for surgery or want to delay it.
- Pain relief is needed to allow participation in rehab or exercise.
However, they may not be suitable for everyone. People with uncontrolled diabetes, certain infections, blood clotting disorders, or severe osteoporosis may not be ideal candidates due to potential risks.
Costs & Insurance Coverage in the UK
NHS – Spinal injections may be available, but waiting times vary.
Private treatment: Costs typically range from £800 to £1,500 per injection, depending on the provider, location, and whether imaging guidance is used. Many Private health insurance policies will cover spinal injections if a consultant deems them medically necessary.
So, Should You Get a Spinal Injection?
It depends (sorry). If pain is stopping you from living your everyday life and other treatments haven’t worked, a spinal injection could be worth exploring. But it’s important to understand that they’re not a magic fix — they will not cure the problem. The best approach is usually a combination of treatments and staying active, doing physical therapy, getting quality sleep, and managing stress (which often worsens pain!).
Final Thoughts
Before making a decision, talk it through with your healthcare provider — whether that’s your doctor, osteopath, or physiotherapist—so you can fully understand the pros and cons based on your situation.
Resources:
-
NHS – Epidural Injections for Back Pain: https://www.nhs.uk/conditions/epidural-injections/
-
British Pain Society – Pain Management Information: https://www.britishpainsociety.org/
-
Versus Arthritis – Steroid Injections: https://www.versusarthritis.org/about-arthritis/treatments/drugs/steroid-injections/
Disclaimer:
Please note that this information is for guidance only and should not be considered a substitute for medical advice, diagnosis, or treatment given in person by a trained health professional.