As mentioned in the main menopause post (read it here), a blood test is generally not required for healthy women over 45 experiencing symptoms linked to perimenopause or menopause. According to the NICE guidelines, a diagnosis of menopause is made based on clinical symptoms rather than blood tests, especially for women over 45. However, checking hormone levels can be important in certain situations, such as for women with concerns about early menopause or to assess the effectiveness of hormone replacement therapy (HRT).
Key Hormones Checked
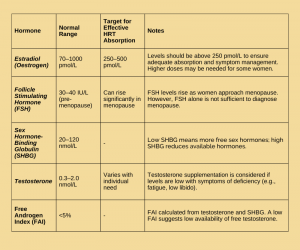
- Estradiol (Oestrogen) Estradiol is the primary form of oestrogen and is measured to check the oestrogen levels in the blood. Estradiol levels can fluctuate significantly during perimenopause and menopause, so while blood tests may not diagnose menopause, they are helpful for monitoring the effectiveness of HRT. The NICE guidelines recommend monitoring estradiol levels in patients using HRT to ensure they are absorbing sufficient oestrogen, particularly if using patches, gels, or sprays. This ensures the dose is adequate for managing symptoms and reducing long-term health risks. Ideal levels for estradiol range from 250 pmol/L to 500 pmol/L for effective symptom relief, although some women may require higher levels. Estradiol levels above 250 pmol/L are generally considered necessary to manage symptoms effectively.
- Follicle Stimulating Hormone (FSH) FSH is a hormone produced by the brain that stimulates the ovaries to produce oestrogen. While FSH levels often rise during menopause, the NICE guidelines state that FSH testing is not recommended for diagnosing menopause in women over 45 who have typical symptoms. However, FSH levels can be helpful in diagnosing early menopause (before age 40) or for women under 45 with abnormal symptoms. Fluctuating FSH levels don’t definitively indicate menopause on their own.
- Sex Hormone-Binding Globulin (SHBG) SHBG is a protein that binds to hormones like testosterone and estradiol, making them unavailable for use in the body. When SHBG levels are high, fewer of these hormones are active. The NICE guidelines recommend checking SHBG levels to get a clearer picture of how much free hormone is available in the body. This test can be beneficial for those on HRT to assess whether the hormone is being correctly utilised.
- Testosterone. Women also produce small amounts of testosterone, which plays a role in energy, libido, and muscle strength. The Free Androgen Index (FAI) is calculated by measuring both testosterone and SHBG levels. A low testosterone level, in combination with symptoms like fatigue, brain fog, low libido, and muscle weakness, may indicate that testosterone supplementation is needed. The NICE guidelines recommend testing testosterone levels to assess this, although supplementation should be considered based on symptoms and overall health, not just hormone levels.
Why Checking Hormone Levels is Useful
Monitoring estradiol levels can help ensure that your HRT is working as it should. Estradiol levels are most valuable when using patches, gels, or sprays, as these forms of oestrogen are absorbed through the skin. This helps confirm that adequate levels are getting into your bloodstream to manage symptoms and protect long-term health, including reducing the risk of osteoporosis and heart disease.
For those experiencing early menopause, it’s important to ensure that estradiol levels are high enough to avoid health complications down the road. If estradiol levels are too low, you may still be at risk for heart disease, osteoporosis, and dementia, which is why sufficient oestrogen levels are necessary. The NICE guidelines support using higher doses of oestrogen in some women to address these risks.
Testosterone levels are not typically measured unless there are signs of testosterone deficiency, such as low energy, mood changes, or low libido. In these cases, checking both testosterone and FAI levels is recommended to help guide treatment decisions.
Normal and Healthy Hormone Levels
To maintain healthy hormone levels, estradiol should be above 250 pmol/L, although some women may require higher levels to achieve symptom relief. The NICE guidelines state that individualisation of treatment is essential, as each woman’s body absorbs and metabolises hormones differently. While normal estradiol levels can range up to 1000 pmol/L, it is not typical for women to go beyond this level without medical supervision.
Testosterone and SHBG levels vary from person to person, but generally, FAI levels should be less than 5%. If you have low testosterone or low FAI, and symptoms suggest testosterone deficiency, supplementation could be beneficial.
The NICE guidelines also support the idea that women may need higher doses of oestrogen than typically recommended to manage symptoms, especially if there are issues with absorption, such as with patches, gels, or sprays.
Checking Hormones While on HRT
NICE guidelines recommend that women using HRT should have regular follow-ups (usually every 3–6 months) to ensure that treatment is effective and to check for any potential side effects. Blood tests for estradiol may be conducted to ensure adequate absorption, particularly if there are concerns about persistent symptoms despite using transdermal HRT. If estradiol levels are lower than expected, adjustments to the HRT dose or delivery method may be necessary. They [NICE] also recommend that hormone levels be monitored at least annually to ensure effectiveness and prevent any imbalances.
Regular testing of testosterone and SHBG levels should also be considered for women on testosterone supplementation, especially if symptoms like fatigue, low libido, or muscle weakness persist.
Hormone Levels for Monitoring HRT Absorption
In conclusion, while blood tests for hormones like estradiol, FSH, SHBG, and testosterone are not typically needed in most women over 45 experiencing perimenopausal or menopausal symptoms, they can be valuable tools when there is concern about early menopause or to monitor HRT effectiveness. The key is tailoring the HRT dosage to each individual’s symptom profile and hormone levels, ensuring optimal absorption and symptom relief.
Disclaimer: This blog is for guidance only and should not replace medical advice, diagnosis, or treatment provided by a qualified health professional. Always consult your healthcare provider for personalised advice and support