The deep, nagging ache in your buttock that sometimes radiates down the back of your leg is undeniably real. But is your piriformis muscle truly to blame, and does “piriformis syndrome” even exist?
What is the Piriformis Muscle?
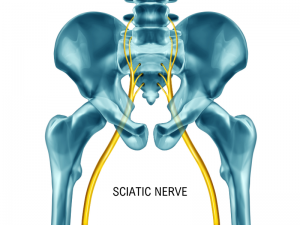
The piriformis is a small but powerful muscle deep in the buttock, running from the sacrum (the triangular bone at the base of the spine) to the top of the thigh bone. It helps rotate the leg outward and stabilises the pelvis during movement. The sciatic nerve—the longest nerve in the body—runs either underneath or, in some cases, directly through this muscle. If the piriformis becomes tight, inflamed, or overworked, it can irritate or compress the sciatic nerve, leading to pain and discomfort.
A Brief History of “Piriformis Syndrome”
The idea that muscle entrapment could cause sciatic-type pain was first suggested in the 1920s. In 1947, British physician Dr Yeoman established a connection between the piriformis muscle and irritation of the sciatic nerve. Then, in 1952, Dr Robinson formally defined the condition now known as “piriformis syndrome.” Over the following decades, awareness of this syndrome increased, particularly within the fields of sports medicine and physiotherapy. However, due to the lack of clear diagnostic tests, some healthcare professionals debate whether “piriformis syndrome” exists or if it even qualifies as a distinct medical condition. and for these reasons, it’s likely to be overdiagnosed, especially during virtual and brief non-examined consultations
What Causes Piriformis Pain?
Piriformis pain can develop for several reasons, including:
- Overuse or repetitive strain – Activities like running, cycling, or prolonged sitting can stress the piriformis muscle.
- Muscle imbalance – Weakness or excessive tightness in surrounding muscles can place extra strain on the piriformis.
- Trauma or injury – A fall, a road traffic accident, or any direct impact can irritate the muscle.
- Poor biomechanics – Sitting for long periods, particularly with a wallet or phone in the back pocket, can contribute to symptoms.
- Spinal Disc problems -Herniated or prolapsed Disc
How to Differentiate “Piriformis Syndrome” from Similar Conditions
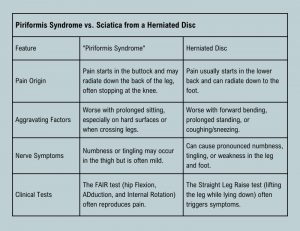

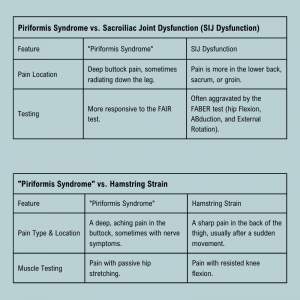
Diagnosis: Is It Really “Piriformis Syndrome”?
There is no definitive test for “piriformis syndrome.” Diagnosis is typically based on symptoms and a physical examination conducted by an osteopath or physiotherapist. Movement assessments, evaluations of muscle tightness, and nerve tests such as the FAIR test can help determine if the piriformis muscle is the underlying issue.
Signs and Symptoms of “Piriformis Syndrome”
- Deep aching pain in the buttock, often worsened by prolonged sitting or activity.
- Pain radiating down the back of the leg, sometimes mimicking sciatica.
- Tenderness when pressing on the piriformis muscle.
- Discomfort when crossing one leg over the other.
Treatment and Management
The good news is that “piriformis pain” is usually manageable with conservative treatment. Here are some approaches that can help:
- Stretching and Mobility Exercises – Gentle stretches targeting the piriformis and surrounding muscles can alleviate tightness.
- Strengthening Exercises – Strengthening the buttock or gluteal muscles and balancing torso strength, aka the core, can improve stability and reduce strain.
- Hands-On Treatment – Osteopathy, massage therapy, or myofascial release can help relieve muscle tension.
- Postural Adjustments – Avoid prolonged sitting on hard surfaces and ensure proper desk ergonomics.
- Heat or Ice Therapy – Heat can relax tight muscles, while ice can help reduce inflammation.
- Nerve Flossing Techniques – Some clinicians recommend specific exercises to decrease nerve irritation.
- Gradual Return to Activity – If movement or exercise triggers symptoms, modifying intensity or incorporating rehabilitation techniques can help.
When to Seek Help
If symptoms persist despite self-care, or if you experience severe pain, leg weakness, or numbness, it is advisable to consult a healthcare professional to rule out conditions such as a herniated or prolapsed disc.
Final Thoughts
For those experiencing deep buttock pain, it can be a frustrating issue made worse by the controversial diagnosis of “Piriformis syndrome.” The good news is that with a careful history and thorough examination leading to a beneficial approach—focusing on mobility work, strengthening, and posture awareness—it is often a temporary setback rather than a long-term problem. Hands-on treatment from an osteopath can provide relief and create a personalised recovery plan.