Just saying the word ‘menopause’ can provoke strong emotional responses: denial, confusion, and sometimes fear. One way to move past these feelings is to have conversations and share knowledge to dispel the many myths and misconceptions about menopause so those experiencing mid-life changes can make informed choices about how to navigate this phase of life.
Like much of the health, fitness and wellbeing industry, there is a cesspool of pseudoscience and misinformation to navigate. Let’s unpack the inside scoop on all things menopause because knowledge is a superpower!
Being menopausal is more than the cliche of a sweating, damp-haired person leaning into a freezer while buying groceries. Your own experience of menopause will differ significantly from other people’s. Some don’t find it a positive or enriching life experience. While some discover newfound freedom, liberated by the end of periods and the risk of getting pregnant, for others, it brings mixed feelings around losing fertility whether they have children or not.
Menopause language and inclusivity
Menopause and ageing are heavily associated with negativity in Western cultures. U.K. mainstream media and the education system are very white-focused, cis-gendered and heterosexual, resulting in menopause conversations and resources that can often exclude the experience of people who are not -white, cis or hetero. Primarily, menopause happens to *cis-gendered women, those who identify with the biological sex they were assigned at birth, but importantly, it [menopause] also occurs in the LGBTQ+ community: trans men, non-binary and intersex folks. Who I do not want to omit or ignore from this conversation.
I know from personal experience that when people don’t use inclusive language, it can be othering and have a damaging impact making the people affected feel ignored or invalidated. However, for ease, I will use “women” when discussing this subject with the intention that it covers all those with female anatomy and who will experience menopause.
Menopause is not a disease.
Menopause is when a woman stops having periods; it marks the end of their fertile years. Periods usually become less frequent over a few months or years before they stop altogether, but sometimes they can stop suddenly.
3 phases of Hormonal midlife
- Perimenopause – anytime from the early 30’s, typically mid-late 40’s
- Menopause – It is one day. The day that marks the end of the last menstrual period or surgical or chemical end of menstruation
- Post-menopausal – The rest of your life without oestrogen!

Menopause, when does it happen?
Menopause is just one day in the calendar, a moment in time, marking 12 months of no periods; before this, you are in perimenopause, and after, you are post-menopausal.
The average age of menopause in the U.K. is 51 for Caucasians, 49 for African, Caribbean or Latino descent and 45-47 years for those from Southeast Asia. It (menopause) can have a challenging effect on all aspects of life; while Western cultures associate menopause with hot flashes, women in other cultures often associate menopause with different symptoms. For example;
- Japanese women report experiencing headaches, shoulder stiffness and chilliness.
- Nigerian women list joint pain as their most common menopausal symptom.
- Filipino women list headaches first and hot flashes last.
- Lebanese women report fatigue and irritability.
- Black and Latina folks report experiencing more vasomotor symptoms, hot flushes and night sweats than white people do, and Latinos experience more vaginal dryness.
Research shows that in addition to Black and Latina women reaching menopause earlier than other groups, they also spend more time in perimenopause than their white counterparts. Dr Nanette Santoro, a professor at the University of Colorado School of Medicine, states that the reasons for this as “lifestyle, socioeconomic status, and other stressors such as systemic racism and their long-term consequences.”
Perimenopause
The shifting hormonal landscape can be subtle and is the first place where myths and misconceptions arise. It is also known as the menopause transition, a hormonal shift journey that eventually leads to menopause. It begins much earlier than most people realise and can start in the late 30s and 40s. Perimenopause lasts up to the point when the ovaries stop releasing eggs. Then, in the last 1 to 2 years of perimenopause, this drop in oestrogen speeds up. The average length of perimenopause is four years, but it may last as little as a few months or continue for ten years.

Perimenopause Symptoms
It’s not uncommon to be told you can’t be perimenopausal because periods are regular; this is a myth. Many people are surprised by unfavourable changes in their mental health or exacerbations of existing psychological and physical health conditions at this time, and misdiagnosis with other disorders is common.
Irregular periods are common and considered normal during perimenopause. However, other conditions can cause changes in menstrual bleeding, so medical assessment should be sort. Please see your doctor rule out other causes if any of the following situations apply to you if your period:
- It is very heavy or includes blood clots.
- It lasts several days longer than usual.
- You have spotting between periods.
- Have spotting after sex.
- Periods occur closer together.
Menopause symptoms
At least 34 commonly reported symptoms are noted in Western society associated with menopause, and up to 48 report worldwide. Hot flushes, or flashes to our U.S. cousins, are probably the most recognisable symptom associated with menopause, and around 75% of Western women experience them regularly. The problem with hot flushes is that they can only sometimes be disguised or hidden from others. Many women say they are “embarrassed” by the clammy, sweaty skin and flushing pink cheeks, which makes them worse.
Hot flushes can also increase heart rate, heart palpitations, perspiration, red and blotchy skin, and sometimes, feelings of nausea, dizziness, and anxiety. The exact cause is unknown, but it is believed to be related to decreased oestrogen levels, causing the body’s natural thermostat, the hypothalamus, to become more sensitive to slight changes in body temperature. As a result, the hypothalamus gets confused, thinking that the body is too warm, but the hot flush occurs in an attempt to cool you down.
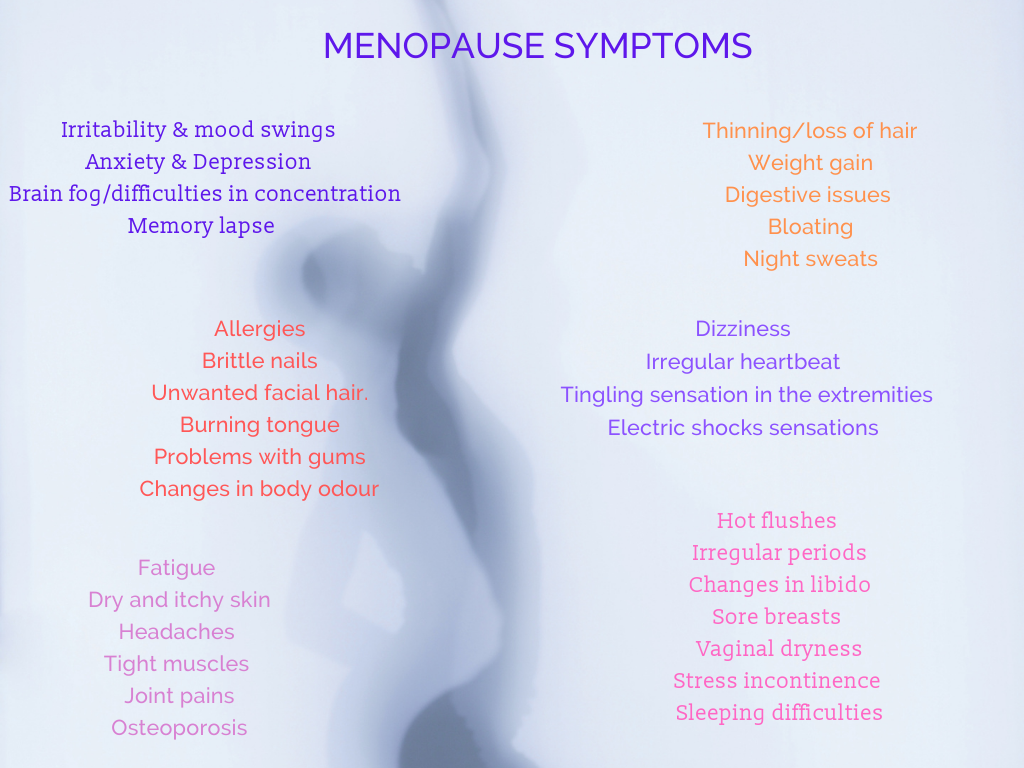
The other common symptom is night sweats, which are effectively hot flushes that occur during the night and often wake folks up from their slumber. These sweats negatively impact energy levels the following day and exacerbate physiological stress, the ability to concentrate, and more.
One of the biggest questions to ask yourself when experiencing night sweats is, did you wake up hot and sweaty, or were you disturbed by something else, and then the body temperature started to rise? In many cases, the night sweat begins after being woken up. The initial disruption to sleep could be something outside your control or a result of blood sugar levels changing, undoubtedly possible if you have eaten sugary foods or consumed alcohol in the evening
Early or Premature menopause
Menopause under 45 is considered early; 40 or younger is considered premature menopause. Early menopause, occurring in women under age 45, is seen in about 5% of women. Premature menopause happens to about 1% of women under age 40. In cases with no apparent medical or surgical cause for premature menopause, such as removing the ovaries or damage to the ovaries from chemotherapy or infection during early menopause, it’s called primary ovarian insufficiency (POI). Primary ovarian insufficiency is also called premature ovarian insufficiency; it affects about 1 out of every 1,000 women ages 15 to 29 and 1 out of 100 women ages 30 to 39.
What causes premature menopause?
Premature menopause can be caused by a medical condition or treatment or may have no known cause (spontaneous). Possible factors that could cause premature menopause include:
- Having surgery that removes the ovaries.
- Being a smoker.
- Having surgery to remove the uterus (hysterectomy).
- A side effect of chemotherapy or radiation.
- Having a family history of menopause at an early age.
- Having certain medical conditions, including:
- Chromosomal abnormalities (Fragile X, Turner’s syndrome).
- Autoimmune diseases (i.e. rheumatoid arthritis, inflammatory bowel disease).
- HIV and AIDS.
- Having certain infections, including Mumps.
Women with primary ovarian insufficiency require HRT (unless there is a contraindication) until at least the average age of menopause, which is 51 in the U.K., to prevent the increased risks of cardiovascular disease, dementia and osteoporosis. They will also usually need and benefit from psychological support.
Postmenopause
Is life after there has been no period for an entire year; menopausal symptoms, due to the continued decrease in oestrogen levels symptoms like vaginal dryness and hot flashes, may linger and, in some cases, continue for a decade or longer. In addition, due to a lower oestrogen level, the post-menopausal phase of life increases the risk of several health conditions, including osteoporosis and heart disease.
Diagnosing perimenopause or menopause
Blood test results are not required, although some people want them, and they may be helpful in some cases, especially in younger people suspected of premature menopause. However, there is a problem; hormone levels constantly change throughout the menstrual cycle, so one-off results will only reflect how hormone levels change at other times of the day, week, or month. As a result, several tests may be required across a cycle to get the complete picture, and that’s expensive and not necessarily helpful.
To clarify, the current guidance, NICE states a “diagnose” can be made without laboratory tests in otherwise healthy women aged over 45 years with the following symptoms:
- Perimenopause based on vasomotor symptoms and irregular periods
- Women who have not had a period for at least 12 months and are not using hormonal contraception
- Based on symptoms in women without a uterus.
Management of adverse menopause symptoms
There are four considerations for current and future health and wellbeing
- Brain
- Bones and soft tissues
- Blood vessels
- Bits and bobs!
NHS management
NICE also states that Drs should explain that, as well as a change in menstrual cycles, folks may experience a variety of symptoms associated with menopause, including:
- vasomotor symptoms (for example, hot flushes and sweats)
- musculoskeletal symptoms (for example, joint and muscle pain)
- effects on mood (for example, low mood)
- urogenital symptoms (for example, vaginal dryness)
- sexual difficulties (for example, low sexual desire)
Give information about the following types of treatment for menopausal symptoms:
- hormonal, for example, hormone replacement therapy (HRT)
- non-hormonal medications
- non-pharmaceutical, for example, cognitive behavioural therapy (CBT)
NICE recommendations
After discussing the short-term (up to 5 years) and longer-term benefits and risks, offer’ women’ HRT for vasomotor symptoms.
Offer a choice of preparations as follows:
- Oestrogen and progestogen to women with a uterus
- Oestrogen alone to women without a uterus.
- Consider vaginal oestrogen after seeking advice from a healthcare professional with expertise in menopause for women with urogenital atrophy in whom systemic HRT is contraindicated.
- Consider testosterone supplementation for menopausal women with low sexual desire if HRT alone is ineffective.
- Do not routinely offer selective serotonin reuptake inhibitors (SSRIs) or clonidine as first-line treatment for vasomotor symptoms alone.
Explain to women that there is some evidence that isoflavones or black cohosh may relieve vasomotor symptoms. However, explain that:
- Multiple preparations are available, and their safety is uncertain.
- Different preparations may vary.
- Interactions with other medicines have been reported.
Stigma
Menopause is still dreaded by many, and sadly, there is still much ambiguity about what menopause means and the best management steps. In the same way that menstruation was once taboo and secret (still is in some parts), the first step towards de-stigmatising and normalising this natural life experience is encouraging people to talk and others to listen without judgment. A report by the Government Equalities Office has criticised employers for their lack of support for menopausal employees. The report estimates that this costs the economy £7.3m annually in absence-related costs. The stigma of menopause, with its associations with incompetence and hysteria, led those affected to report feeling at risk of ridicule and ageism and the taboo about revealing menopausal symptoms, causing some female employees in their early 50s to call in sick for fear of experiencing symptoms at work.
More in part two, including-
- HRT, benefits and risks
- Alternatives to HRT.
- Resources
In the meantime, if perimenopause, menopause or post-menopause symptoms negatively affect the quality of your life, please speak with your GP or seek support from a gynaecologist.