Fibromyalgia is a mysterious long-term condition involving widespread chronic pain without a known cause; it’s more frustrating than a diagnosis. Some people will eventually discover a specific reason. Still, most times, the condition appears triggered by a physically stressful event, such as an injury, infection or having a baby. Or an emotional upset, such as bereavement or a relationship breakdown.
Also called fibromyalgia syndrome (FMS), it affects 2–4% of the population. It can occur at any age, in both sexes, but most commonly in women, typically developing between 3 and 50.
What causes it?
Research suggests Fibromyalgia is not an autoimmune or inflammation illness but one where the brain has a problem interpreting pain signals from the nervous system. Still, all medical practitioners do not fully understand or recognise the condition. It is often misdiagnosed by healthcare professionals and misunderstood by the public.
Background and history
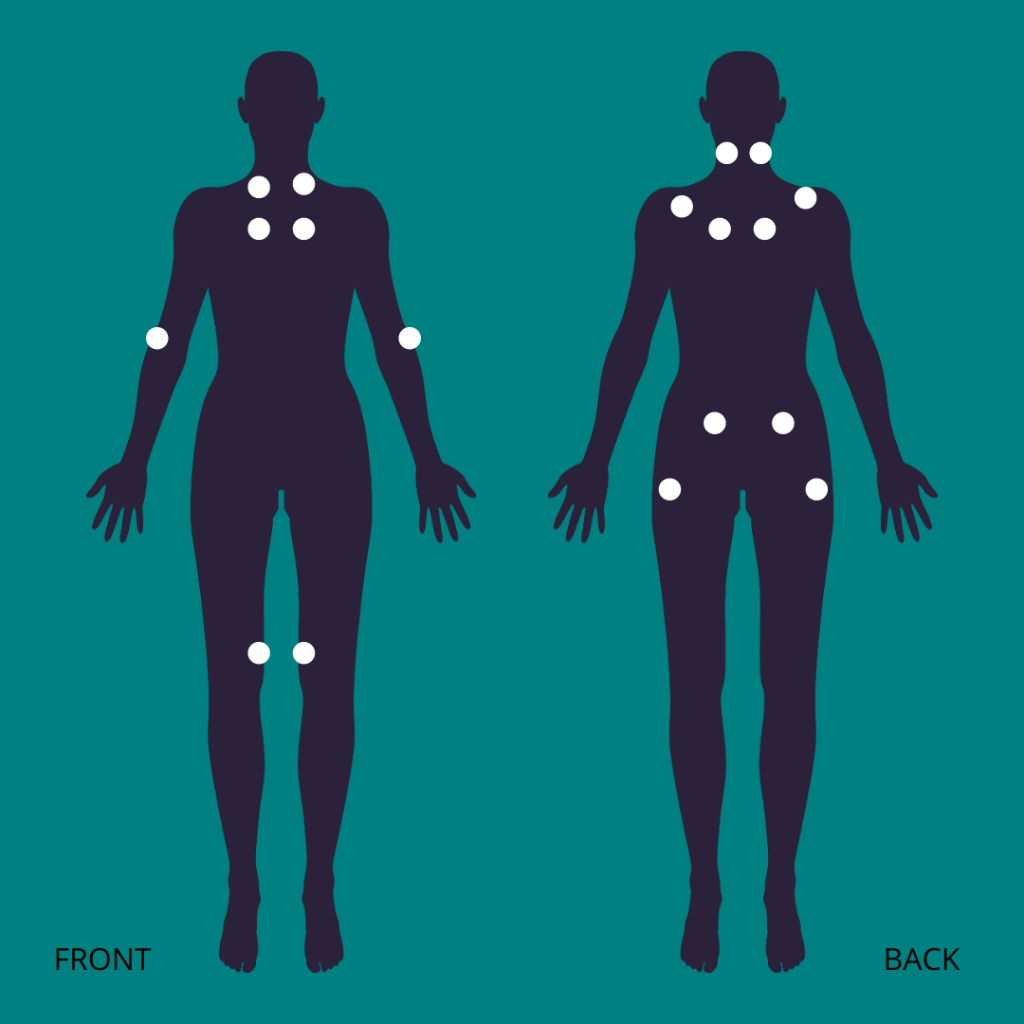
Fibromyalgia is not a new condition; it’s existed for centuries and was once considered a mental disorder until the tender points associated with it were discovered in the early 1820s. It was then reclassified as fibrositis because the pain was believed to be caused by inflammation at the tender sites.
In 1976, it was renamed Fibromyalgia, derived from the Latin word “fibro” (fibrosis tissue) and the Greek terms for “myo” (muscle) and “algia” (pain). In 1981 Dr Muhammad Yunus, known as “The Father of Fibromyalgia”, published his first paper. The International Diagnostic Criteria for Fibromyalgia were clarified in 2019 to include the following:
- A 3 months history of pain
- With severe pain in 3 to 6 different body areas or milder pain in 7 or more different areas. Note: this is assessed by applying gentle pressure to specific “tender points” where the pain is likely to be at its worst.
- Moderate sleep disturbance
- Fatigue
- No other reason for the symptoms has been determined.
Symptoms
Fibromyalgia can feel similar to other joint-related problems, such as osteoarthritis and tendinitis, but the symptoms are more widespread throughout the body than in a specific area. They also come and go for no apparent reason and move around the body; symptoms can include:
- Muscle pain or tight, tender spots
- Debilitating fatigue
- Burning sensation or muscle, twitching
- Numbness or tingling in the arms, hands, legs, feet, and face.
- Difficulty concentrating, aka “fibro fog.”
- Insomnia or poor quality, un-refreshing sleep
- Feeling nervous, worried, or depressed.
- Sensitivity to cold, heat, light, or sound
- Headaches or head pain
- Digestive symptoms: abdominal pain, nausea, bloating, and IBS (irritable bowel syndrome), including constipation and diarrhoea.
- Dry mouth and eyes
- Urinary frequency
Risk factors include people who also have the following:
- Other painful conditions such as lupus, rheumatoid arthritis, or ankylosing spondylitis.
- A family member with the condition.
- Anxiety, depression, or another mood disorder.
- A sedentary lifestyle and rarely exercising.
- A previous history of abuse (physical or emotional) or living with PTSD.
Getting a diagnosis
There is no test for Fibromyalgia, so diagnosis is made following a careful medical history and physical examination and by elimination. Blood tests are usually needed to rule out other conditions, check hormone levels and look for signs of inflammation.
Other considerations
- Myofascial pain syndrome
- Autoimmune conditions such as multiple sclerosis, lupus, and ankylosing spondylitis, especially in the early stages
- Hypothyroidism
- Vitamin D or B12 deficiencies
- Coeliac disease
- Myelopathy resulting from spinal cord compression
- Mood disorders, including depression and anxiety disorders
- Lyme disease
- Myalgic encephalomyelitis (also called, inaccurately chronic fatigue syndrome)
Treatment
There is no known cure for Fibromyalgia, but medication can reduce symptoms in some people. Treatment plans usually involve a combination of medications such as painkillers, antidepressants and graded exercise. Plus, support or talking therapies to manage stress and mood therapies.
Lifestyle, mind, and movement
Lifestyle changes may ease symptoms and enable people to live more active, meaningful lives. Stress reduction is fundamental to any fibromyalgia treatment plan; relaxation techniques and mind-body therapies can be effective options because they help release “feel-good” chemicals: serotonin, dopamine, and endorphins.
Meditation, mindfulness, guided imagery, and deep breathing are valuable options too. While ‘pacing’ is key to managing symptoms, do not overdo it by balancing periods of activity with rest. Adding in movement practice, such as restorative pilates or yoga, Tai Chi or Qi Gong, is an excellent way to build resilience. The controlled movements of these methods help release tension but shouldn’t cause fatigue.
Summary
Fibromyalgia is a long-term condition that, in a few cases, results in disability. Treatment is most effective when an integrative approach is used, one that includes patient education, exercise, and medications. People affected respond best with multifactorial healthcare approaches.
Support
Fibromyalgia Action UK is a charity that offers information and support groups. Some people find this a helpful network where they can talk to others with the condition.